The Vulnerable
Why actuaries need to develop new tools, techniques and insights to provide a reliable guide to navigate the effects of future climate developments
April/May 2018Statements of fact and opinions expressed herein are those of the individual author(s) and are not necessarily those of the Society of Actuaries or the respective authors’ employers.
Climate change will have a wide-ranging global impact. Future changes will in some way impact the population of all countries and in all socioeconomic categories. These impacts include health and quality of life, property and the environment—with dramatically diverse results by geographic area and population segments. One important type of impact worthy of study is the mortality of the population, which is the focus of a paper1 made available in November 2017 by the International Actuarial Association’s Working Group on Resources and Environment.
The climate process is complex and ever changing. It is made up of many elements, including temperature, humidity and precipitation. The long-term trends involved will continue to affect many aspects of human life, both directly and indirectly.
The analysis of and actions related to the process of climate change, from causes to potential damages, is a perfect example of a social risk management process. The process includes the study of underlying causes; for example, greenhouse gas emissions, the interrelationship between these causes and damages, the analysis of economic/actuarial damages, and possible mitigation and adaptation actions. The remainder of this article will examine this process with respect to mortality damages.
It is useful to categorize its impacts into sudden and slow onset types. Examples of the former are storms, heat surges and extreme weather events; examples of the latter include sea level and water quality, desertification and deglaciation. Although it is common to focus on these big news developments, often the secondary and indirect effects can be just as crucial in climate impact assessments and also need to be addressed.
There are many contributing factors affecting long-term weather patterns. Scientific observations have shown that the relatively recent (over the last 150 years, but especially the last 50 years) and continuing increases in accumulated greenhouse gases (e.g., carbon dioxide and methane) in the atmosphere and oceans contribute to some fairly radical changes in long-term climate effects.
The Vulnerable
The at-risk populations are especially important to examine. Those particularly vulnerable to mortality risk differ by each of the dimensions of climate change (see Figure 1 for key examples). Those most at-risk of excess deaths due to disease tend to live in zones closer to the equator, coincidentally where the weakest health infrastructure exists. Those most at-risk due to heat-stress tend to live in areas more exposed to seasonal heat surges (those in areas used to cold conditions may benefit from higher temperatures, while the non-vulnerable living in hotter conditions all year long have steeled themselves to excessive heat already). Although those living next to an ocean will be exposed to gradual sea level rise, those who can afford to should have sufficient time and resources to prepare for it; excess mortality risk will tend to be of a secondary or tertiary nature that occurs primarily after emigration from the coast.
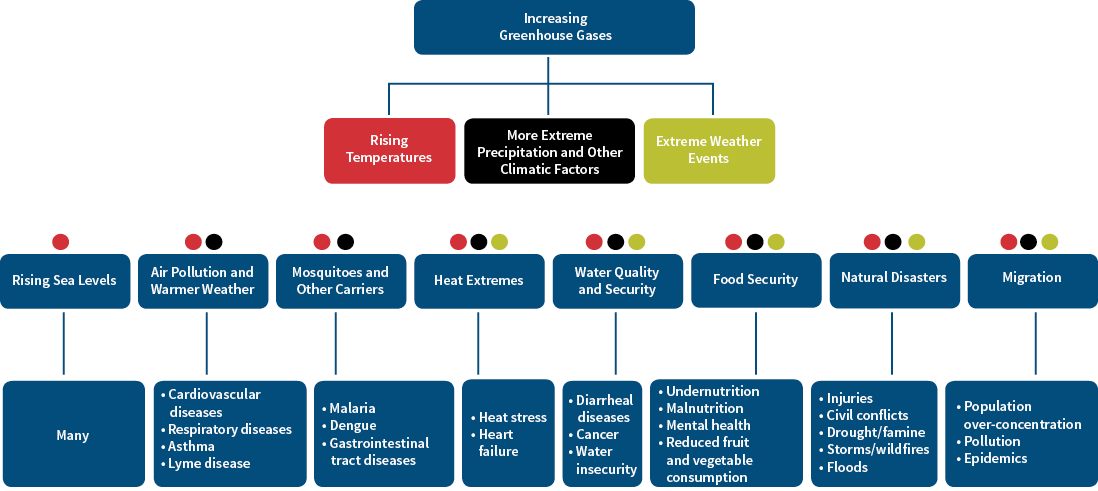
Figure 1: Adverse Effects on Mortality From Climate Change
Vulnerable populations often have access only to at-risk medical infrastructure (this infrastructure may be weak in the first place), with no accessible backup to provide for times of extreme health risks. This creates or exacerbates the risk to these vulnerable populations. This risk was experienced during the immediate aftermath of Hurricane Katrina in Louisiana in 2005.
Those who are less well-off may be adversely affected partly because they have less access to affordable living conditions and support. For example, when drought, famine, sea level change, conflicts or other extreme conditions occur, they may not be able to afford to move into non-at-risk areas or housing. Housing and access to proper medical care for those with low or no income tend to be of poor quality, with resultant exposure to disease and malnutrition. Those with lower income cannot afford to live or work in resilient structures. Even after a natural disaster occurs, due to affordability concerns, they will often just move back and re-expose themselves to the same hazard.
The very oldest and youngest members of a population may be most at risk to many mortality hazards emanating from climate change. The frail will often be among the most affected in times of weather extremes, particularly in heat surges where the elderly are among the most vulnerable. The youngest who are most at-risk to such climate-related conditions such as diarrheal disease and food insecurity will experience stunting, arising from malnutrition.
Climate Change
Two major elements of climate are temperature and precipitation:
- Temperature. This is most commonly referred to in this context as global warming. Possibly the most advertised effect of climate change is the effect on average and extreme (volatile) temperatures, influencing many facets of air, water and land surface temperatures. The frequency of extreme heat has become increasingly common, as well as decreases in extreme cold. It appears that in recent decades both record average global temperature and heat waves have become more common.2 Warmer temperatures increase water evaporation, while warmer water can increase the severity of extreme storms such as hurricanes, whose genesis or trajectory is over an ocean.
- Precipitation. Changes in precipitation can lead to more intense individual downpours or drawn-out drought conditions. Excessive precipitation can result in flooding and soil erosion with deadly results. Droughts in already arid regions may continue in duration and may spread and increase in severity. Water scarcity in areas in which vulnerable populations reside will adversely affect human health and mortality. These very different climate patterns will vary by geographic area and may vary by time period.
Humidity, barometric pressure and ultraviolet radiation that reach extreme and damaging conditions will add to the harm, especially when acting together. For example, drought conditions have caused significant public health catastrophes, resulting in mass migration, malnutrition, poor living conditions and increased deaths in areas such as Eastern Africa. Although short-term exposure can be bad enough, adverse results from multiyear drought conditions are not restricted to what people drink. They also extend to what is eaten, as the human activity that consumes the most water is agriculture, the source of income and food to many.
Although many think of climate change in terms of something that will start snowballing sometime in the distant future, some of its effects are already upon us. Increases in both the frequency and severity (including their financial effects, which will increase in the future as populations both increase and become further urbanized) of extreme natural events appear to be present already and will likely continue to worsen. These include tropical cyclones (although the frequency of landfall in North America may not increase), tornadoes, floods, windstorms, wildfires, drought (in extremes—famines) and heat waves. These not only affect mortality, but also can cause infrastructure and property damage, with consequential injuries and sickness.
Mortality Consequences
The World Health Organization (WHO)3 estimated that some 12.6 million deaths globally are attributable to the environment (overall—not restricted to that due to climate change), which is about 23 percent of all deaths. Clearly environmental deaths need to be assessed.
Some premature deaths have been shown to be directly due to climate change, while others are indirect consequences (both included in Figure 1). In almost every recent assessment of what seems to be an increasing frequency of natural disasters around the world, an ever-present question is: What is the contribution of climate change to the resulting damages? The developing scientific field of attribution analysis is attempting to answer this question.
Although there is insufficient space in this article to dig into the details of this type of analysis, it is anticipated that as our climate continues to change, this type of questioning will remain important, in part to spur public and private sector involvement in efforts to mitigate and adapt to the changes that will inevitably occur. Although many premature deaths will be due to climate change, certainly the percentage will differ dramatically by cause.
The challenges in estimating these percentages is partly the result of the wide and complex range of interacting causes and effects of climate, which differ by area and population segment. An example is the ever-changing patterns of disease from sources such as certain strains of mosquitoes, drought and famine, conflicts, storms and wildfires, and slow-onset conditions that in turn may lead to migration of vulnerable populations and to high population densities. The process and adverse factors involved are summarized in Figure 1, starting from first-order factors in the first and second rows to the first-order effects in the third row and immediate causes of death and ill-health in the last row. There are significant interactions among the factors in the second row and between the factors and their effects in the third and fourth rows.
Diseases that have been shown to be affected or caused at least in part by climatic factors include:
- Diarrheal diseases. Many deaths are due to low water quality, especially affecting children under the age of 15. By 2030 the WHO4 expects 48,000 annual deaths, especially in Southern and Eastern Asia.
- Malaria and dengue. These diseases are derived in part from increased temperature, which in turn increases the frequency of mosquito bites. By 2030 the WHO expects about 60,000 annual deaths to be due to climate change, offsetting what until recently has been a significant decrease in deaths due to these causes.
- Gastrointestinal tract illness and infection. The number of these deaths in part has been driven by increased water temperature.
- Asthma. Increased temperature, humidity and dust (from droughts and erosion) contribute to increased pollen, mold and air pollution, with resultant increased deaths.
- Cardiovascular and respiratory disease. Increased temperatures and their volatility will contribute to deaths due to heat stress and air pollution, particularly affecting the aging population.
- Cancer. Deaths due to climate change will in part be due to increased ultraviolet radiation.
The United Nations Office for Disaster Risk Recovery (UNISDR)5 expects about 38,000 deaths in 2030 (about 95,000 in 2050) from natural disasters, especially among the elderly. Half of these are expected in Southern and Eastern Asia, with about 10 percent in high-income countries. Alan Barreca6 found that, in the United States, each additional day of extreme heat (more than 90 degrees Fahrenheit) increased mortality by about 0.2 deaths per thousand, or about 0.02 percent, while reported mortality effects of extreme cold appear to be driven more by low humidity than by cold temperatures.
It is important to note that, although many additional deaths are directly and indirectly attributed to climate change due to extreme weather conditions, not all are. Although adverse trends are generally associated with extremes, some of the worst mortality effects are associated with moderately adverse trends. Based on an extensive search of the literature, a 2015 article in The Lancet7 found that, despite the attention given to extreme weather events, most of the effects happened on moderately hot and moderately cold days, especially moderately cold days. The percentage contribution of hot/cold conditions differs dramatically by country and even within countries.
Secondary/Indirect Effects
The direct effects on mortality can be bad enough, but the secondary effects can be killers as well. They include:
- Air pollution. Some of the same contributing causes of climate change also affect the severity of air pollution; warm weather can also increase its health impact. A 2015 article in the journal Nature8 estimated that premature deaths worldwide from outdoor air pollution will increase from 3.3 million per year in 2010 to 6.6 million per year by 2050 (about 12 percent of total deaths) if nothing is done to improve air quality. The main sources of CO2 emissions (e.g., the extraction and burning of fossil fuels) are key drivers of both climate change and air pollution. Based on an experience study of the U.S. Medicare population from 2000 to 2012, a 2017 article9 found that short-term exposures to small particle pollution and warm-season ozone were significantly associated with increased risk of mortality. This risk exists at levels below current national air quality standards, suggesting that these standards may need to be reevaluated.
- Food and water insecurity. One of the most substantial health effects of climate change is expected to be undernutrition and malnutrition causing 95,000 deaths per year in 2030, according to the WHO. However, “Global and Regional Health Effects of Future Food Production Under Climate Change: A Modelling Study”10 indicated that the composition of future diet may have a greater impact than all the climate factors considered by the WHO combined. Twice as many climate-related deaths were associated with reductions in fruit and vegetable consumption than with climate-related increases in the prevalence of malnutrition. Undernutrition and malnutrition at an early age can have long-lasting effects, including increased risk of illness and delayed mental development and premature death, which in turn can be passed on to the next generation.
- Severe weather conditions. Climate change has contributed to the severity of many, but certainly not all, natural disasters.
As with direct causes, it is not claimed that all of these deaths are due to climate change. Nevertheless, many (or the same underlying causes) can be attributed to it.
Favorable Effects
Not all the effects of climate change are adverse. Beneficial effects can also occur as a result of direct climate change itself (e.g., warmer winter temperature may reduce the number of cold-related deaths, more efficient agriculture due to warmer temperature or changing crop patterns may reduce food insecurity in some areas) and from mitigation activities (e.g., increased use of air conditioning may reduce deaths resulting from extreme heat conditions).
In addition, co-benefits may arise from the efforts to adapt to climate change. For example, many deaths have been spared as a result of enhanced planning in anticipation of some aspects of climate change. It has been estimated that there were almost 15,000 deaths in Paris associated with its heat wave in 2003. Comparable heat waves were experienced in the subsequent decade, but fewer deaths resulted because of better preparedness of the public, health infrastructure and enhanced emergency procedures. The moral is that some of the adverse consequences to climate change can be offset by effective mitigation programs, which may also be accompanied by co-benefits.
Quantitative Analysis
Modeling the possible impacts of climate change and different future climate scenarios on future levels of mortality presents formidable challenges, in part due to the interconnected nature of the systems and the uncertainties. Both stochastic modeling and scenario analysis (stress testing for the tails) can provide valuable insights into the extent and characteristics of the populations primarily affected.
It is anticipated that many risks associated with climate change will increase over tiime. As a result, more of the effects on mortality will be felt by most insurance and pension plans over the long term, rather than during the immediate future. The adverse mortality effects may not be as noticeable as those from other factors, although some will tend to occur in bunches (offering an excuse to discount or ignore them as outliers) significantly affected by concentration risk, especially in areas of the world where those who are vulnerable reside.
Two main methods have been used to study the effect of heat stress:
- Study of specific causes of death directly attributed to heat stress, especially of the period immediately after the stressed conditions. Due to the difficulty in obtaining this type of information, this approach’s results may understate the resulting number of deaths.
- Statistical analysis of trends in or excess of seasonal or situational all-cause mortality. Although many other factors can influence the number of these excess deaths, the correlation and trend over time between such excess deaths and extreme temperature condition can provide useful insight into its effects.
A case study in the International Actuarial Association (IAA) paper that is the basis for this article addresses the effects on mortality of warmer temperatures in the United Kingdom. Its conclusion is that fewer deaths may result from climate change in the United Kingdom, as the favorable effect of warmer winters may more than offset the adverse effect of hot summers. A major benefit of this case study is the analytical process described—a rigorous application of the scientific method.
However, the IAA paper also points out that the U.K. findings cannot be generalized. Various studies have indicated a net increase in deaths will be likely in much of the rest of Europe. In areas of the world such as India, a significant adverse mortality risk exists—over the last 50 years a substantial increase in mass heat-related deaths (100+ deaths) has occurred. With increased urbanization, the severity of the impact of extreme events has increased. A 2017 report shows that between 2000 and 2016, the number of people exposed to heat wave events increased by about 125 million people.11 This will remain a problem.
It is also important to realize that in certain parts of vulnerable populations, such as the frail elderly and the disabled, some of the deaths associated with climate change (due to, for example, heat surges) may simply be deaths that have moved forward or been “displaced” by a matter of a few days or months.
Why Should Actuaries be Concerned?
Since most of the areas in which actuaries are more active (e.g., private and public sector insurance, annuity and pension programs) tend to focus on what are considered to be nonvulnerable populations, the direct effect on mortality in these programs may not be as significant as for the entire population, especially its most vulnerable segments. In addition, other factors, including changes in medical treatment and infrastructure, lifestyle and aging, will likely have a far greater effect on mortality than climate change in most population segments where actuaries are involved.
A great deal of uncertainty exists with respect to climate change—not regarding whether climate change exists or who is responsible, but to the extent, timing and severity of resulting damages. This uncertainty arises due to the fact that we have not experienced the types of climatic conditions that may arise and the effectiveness and timeliness of future human intervention. Many aspects of climate change are difficult to estimate; examples include hurricane trajectories, severity of famines, speed of deglaciation and climatic feedback loops, especially caused by clouds. Especially uncertain is the volatility of damages, due to the ultra-long time horizon involved and low-frequency/high-severity nature of some of the possible tail risks. Unfortunately, most new insight has led to more adverse projections.
This is clearly an area in which actuaries need to develop new tools, techniques and insights, as extrapolating historical trends will not provide a reliable guide to future developments. Detailed work will be required both in developing such tools for global use by the profession, and at the local level in applying them to the analysis of the specific set of circumstances of a region or area. It is especially challenging because of the difficulty in interpreting historical experience (due to widely diverse conditions) and inconsistency in reporting around the world.
In conclusion, for many population segments that benefit from actuarial work, the short-term impact will likely be limited and will be overwhelmed by other mortality risks. Nevertheless, in some markets and countries with significant vulnerable populations, the direct and indirect effects may be substantial. As these broader effects of climate change become more observable and more important in overall risk management, actuaries, as professionals and members of society, will be increasingly asked to assess the effect on the risks where actuaries are involved. Our clients will want to enhance their understanding of the impact of climate change on their businesses, so actuaries will need to keep on top of future developments. It demands future research and consideration.
Editor’s Note: This article is based on an International Actuarial Association (IAA) Working Group Discussion Paper.
References:
- 1. Resources and Environment Working Group of the International Actuarial Association. 2017. “Climate Change and Mortality.” International Actuarial Association. November. www.actuaries.org/ClimateChange&Mortality. ↩
- 2. Actuaries Climate Index. 2018. http://actuariesclimateindex.org/home. ↩
- 3. Prüss-Ustün, A., J. Wolf, C. Corvalán, R. Bos, and M Neira. 2016. “Preventing Disease Through Healthy Environments: A Global Assessment of the Burden of Disease From Environmental Risks.” World Health Organization. ↩
- 4. Hales, Simon, Sari Kovats, Simon Lloyd, and Diarmid Campbell-Lendrum (eds.). 2014. “Quantitative Risk Assessment of the Effects of Climate Change on Selected Causes of Death, 2030s and 2050s.” World Health Organization. http://www.who.int/globalchange/publications/quantitative-risk-assessment/en. ↩
- 5. United Nations Office for Disaster Risk Recovery. 2016. “The Human Cost of Weather Related Disasters: 1995–2005.” Centre for Research on the Epidemiology of Disasters. ↩
- 6. Barreca, Alan. 2012. “Climate Change, Humidity and Mortality in the United States.” Journal of Environmental Economics and Management 63 (1): 19–34. ↩
- 7. Gasparrini, A., Y. Guo, M. Hashizume, E. Lavigne, A. Zanobetti, J. Schwartz, A. Tobias, et al. 2015. “Mortality Risk Attributable to High and Low Ambient Temperature: A Multicountry Observational Study.” The Lancet 386 (9991): 369–375. doi:10.1016/S0140-6736(14)62114-0. ↩
- 8. Lelieveld, J., J.S. Evans, M. Fnais, P. Giannodeki, and A. Puzzer. 2015. “The Contribution of Outdoor Air Pollution Sources to Premature Mortality on a Global Scale.” Nature 525 (September): 367–371. ↩
- 9. Di, Qian, Lingzhen Dai, Yun Wang, Antonella Zanobetti, Christine Choirat, Joel D. Schwartz, and Francesca Dominici. 2017. “Association of Short-term Exposure to Air Pollution With Mortality in Older Adults.” Journal of the American Medical Association 318 (24): 2446–2456. doi:10.1001/jama.2017.17923. ↩
- 10. Springmann, M., D. Mason-D’Croz, S. Robinson, T. Garnett, H. Charles, J. Godfray, D. Gollin, et.al. 2016. “Global and Regional Health Effects of Future Food Production Under Climate Change: A Modelling Study.” The Lancet 387 (10031): 1937–1946. ↩
- 11. Watts, Nick, Markus Amann, Sonja Ayeb-Karlsson, Kristine Belesova, et al. 2018. “The Lancet Countdown on Health and Climate Change: From 25 Years of Inaction to a Global Transformation for Public Health.” The Lancet 391 (10120): 581–630. http://dx.doi.org/10.1016/S0140-6736(17)32464-9. ↩


 The very oldest and youngest members of a population may be most at risk to many mortality hazards emanating from climate change.
The very oldest and youngest members of a population may be most at risk to many mortality hazards emanating from climate change. As these broader effects of climate change become more observable and more important in overall risk management, actuaries will be increasingly asked to assess the effect on the risks in areas where they are involved.
As these broader effects of climate change become more observable and more important in overall risk management, actuaries will be increasingly asked to assess the effect on the risks in areas where they are involved.