Precision Medicine Development Process
Solutions to help manage the cost of specialty drugs for gene and cell therapies
February 2021Photo: iStock.com/koto_feja
Precision medicines (e.g., gene and cell therapies) will soon become the biggest driver of specialty pharmacy cost growth, and thus will be one of the biggest contributors to the 18|11 gap. So how do these treatments get discovered and developed? And why are they so expensive?
The process used to develop traditional drugs was discussed in the “Traditional Drug Development Process” article published in May 2020. As a follow-up, this article now provides background on the research and development of precision medicines in contrast to traditional drugs.
As we review the development process of precision medicines, it is helpful to consider the subcategories of biologic drugs, including monoclonal antibodies, gene therapy and cell therapies (see Figure 1).
Figure 1: Specialty Drugs and Biologics
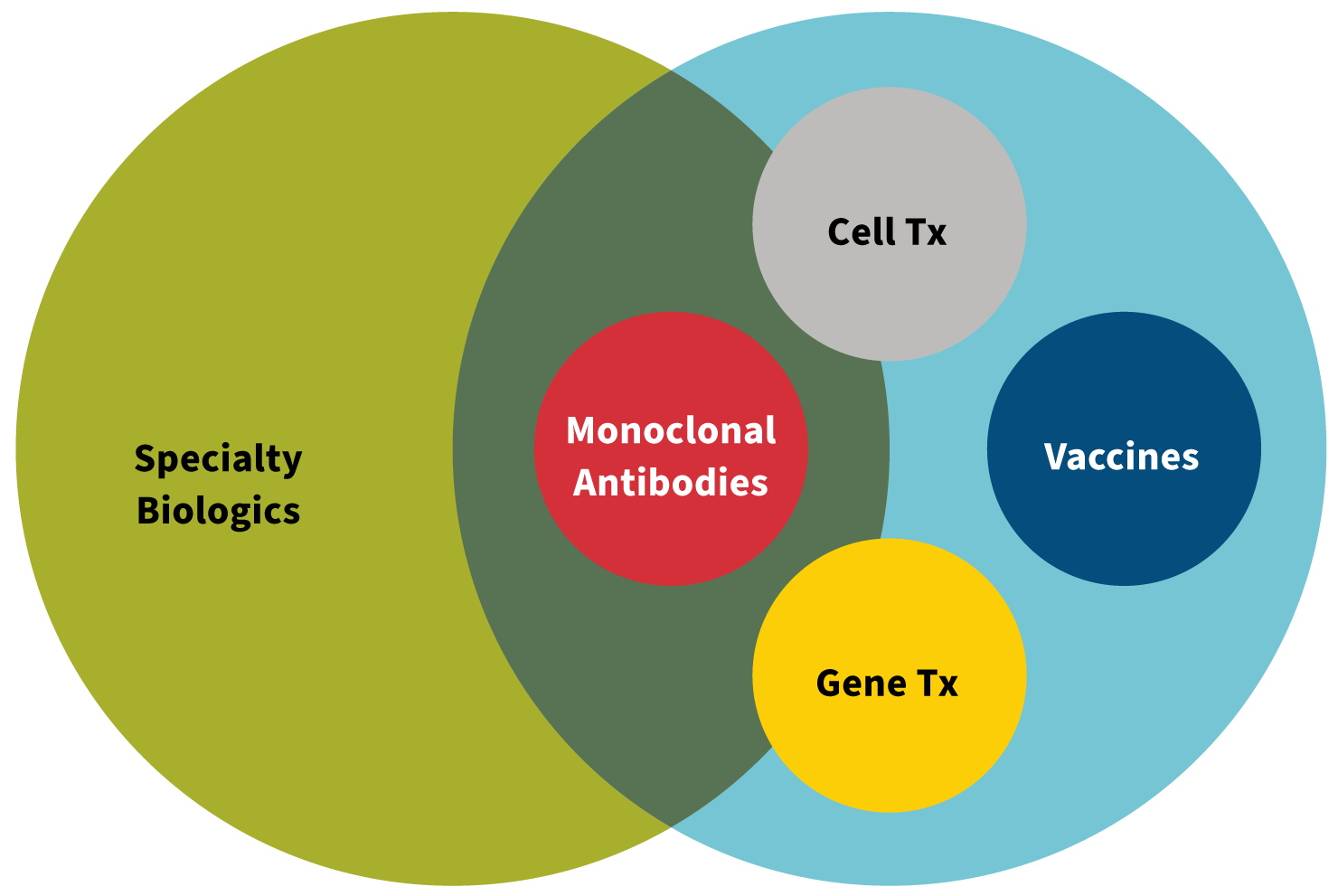
Source: Created by Kerri Miller, Pharm.D.
As science evolves and new technology is discovered, biologic drug development (and even some traditional drug development) becomes more targeted and focused—not only for a specific disease, but in some cases, for specific patients with unique genetic makeups. The development of drugs to target very specific genetic characteristics or mutations is called precision medicine. The different subcategories of biologics are described throughout this article, along with if or how each subcategory fits into the precision medicine of the future.
Cell Therapies
Although it may seem as if cell therapies are relatively new within the armamentarium of treatments for various diseases and conditions, in fact, the routine use of cell therapy has been around for decades. The process of transfusing red blood cells from a donor to a patient is perhaps one of the earliest and simplest forms of cell therapy. Another common historical form of cell therapy is bone marrow transplantation, where stem cells from a donor’s bone marrow are transplanted into a patient’s bone marrow as a treatment to correct an abnormality or deficit in that patient. In today’s environment of the COVID-19 pandemic, cell therapy with convalescent plasma from fully recovered COVID-19 patients has received a great deal of attention and is actively under investigation as a potential treatment for individuals who are seriously ill from the virus.
The three examples just described all have the cells originate from a donor (called allogeneic cells). However, the cells used in cell therapy can also originate from the patients themselves (called autologous cells). Provenge is an example of an autologous cell therapy designed to stimulate a patient’s own immune system against cancer.
In recent years, however, the terms “cell therapy” and “gene therapy” have become intermingled. To explain the two unique concepts, let’s start with a basic question: How do cell therapy and gene therapy differ? The American Society of Gene & Cell Therapy provides this perspective: “Gene therapy involves the transfer of genetic material, usually in a carrier or vector, and the uptake of the gene into the appropriate cells of the body. Cell therapy involves the transfer of cells with the relevant function into the patient.”1
Some drug development protocols utilize both cell therapy and gene therapy, which may be the reason for some gray area in the understanding and distinguishing between the two. In today’s nomenclature, when drugs are described as cell therapy, it is frequently in reference to genetically modified cell therapy. CAR T-cell therapies (such as Yescarta and Kymriah) are examples of genetically modified cell therapies and can certainly be classified as precision medicine. To better understand the genetic modification component, it’s best to dive into the basics of gene therapy.
Gene Therapies
In the broadest sense, gene therapy delivers genetic material to a patient through one of the following mechanisms:
- Adding a gene that has been lost
- Replacing a defective gene with a corrected gene
- Adding a new gene to treat a disease2
The transferred genetic material changes how a single protein or group of proteins is produced by the cell. Gene therapy can be used to reduce levels of a disease-causing version of a protein, increase production of disease-fighting proteins or to produce new or modified proteins.
Since genes are made of DNA, gene therapy requires the transfer of DNA into human cells to work. Cells will not automatically absorb new DNA, so a transport mechanism is needed. For DNA delivery, the transport mechanism is called a vector. Scientists have learned to harness a vector that has proven to be very effective and efficient at delivering foreign genes into cells: the virus. Multiple different types of viruses can be used to deliver the gene, and viruses differ in how well they transfer genes to cells and to what degree the cell’s DNA is altered.3
The main concerns that come with using viral vectors include safety, immunogenicity and manufacturing limits. Nonviral vectors have been developed as an approach to minimize these concerns. Luxterna was the first directly administered gene therapy the Food and Drug Administration (FDA) approved. It uses a viral vector to deliver a normal copy of a specific gene directly to cells in the retina of the eye to restore vision in children with a genetic retinal disorder.
Not only are there different types of delivery mechanisms for gene therapy (i.e., vectors), there are two different environments in which the DNA is transferred into a group of cells in the patient’s body. When a vector (along with the new genetic material) is injected directly into the patient, it is called in vivo (inside the body) delivery. The in vivo process has its challenges, which include triggering the immune response and ensuring the new genetic material reaches the targeted cells. The alternative process is to extract specific cells from the patient’s body and then incorporate the new gene into those cells that are multiplying in culture in the lab. Once there are enough of the new cells with the new gene, they are then put back into the patient—thus taking us back to the genetically modified cell therapy concept. Again, this is a clear connection to precision medicine.
Precision Medicine Cost
The average monthly supply for a traditional brand-name drug is several hundred dollars in total cost (shared by the patient and payer). For specialty brand-name drugs, the average monthly supply can cost several thousand dollars. For precision medicines, the average monthly cost can be tens of thousands of dollars, or even hundreds of thousands of dollars. The drug Zolgensma, a gene therapy treatment for spinal muscular atrophy, made headlines in 2019 as the most expensive drug ever approved by the FDA at $2.1 million for a one-time treatment. By 2025, the FDA estimates that 10 to 20 cell and gene therapy products will be approved each year.4
There are new solutions being developed in the marketplace to help manage specialty drug spend, especially when it comes to cell and gene therapies.
- In Express Scripts’ Embarc Benefit Protection program, health plans pay a fee per member per month (PMPM), and in turn the expense for certain high-cost drugs is covered by the program.5
- Prime Therapeutics’ PreserveRx is a similar program that offers health plans protection from high-cost gene therapy drugs for a PMPM fee.6
If viewed as a pure reinsurance type of arrangement with no other cost reduction efforts, which these programs may have, the health plan may experience a more stabilized and predictable drug spend. But in the absence of specific cost reduction programs, the actual cost still occurs and is merely transferred to various entities.
Another type of solution is value-based contracting. This type of arrangement ties the price paid for the drug to its effectiveness. This may prevent health plans and patients from paying for a treatment that costs hundreds of thousands of dollars (or more) while having a less than optimal clinical outcome.
The crux of the issue is that research and development costs for drugs for these smaller populations have lower volumes across which to be spread, causing per-unit or per-patient costs to often be much higher than those of traditional medications. Managing future drug spend could be viewed as a distribution of the possible expense. One parameter is variation. This trend could cause a wide variation in drug spend, especially for smaller groups if they happen to have a disproportionate number of members requiring these treatments. A drug that costs $1 million (or more) to be administered today may prevent a lifetime of costly treatments, and over the next decade, we will witness how the net effects unfold.
Role Actuaries Can Play
Clearly, actuaries can contribute to this societal challenge through the creation and financial management of risk-bearing solutions such as the carve-out, reinsurance and value-based contracting concepts discussed in this article. But actuaries also can contribute earlier in the development process by helping manufacturers model the potential market need for and impact of various types of therapies and thereby help guide resource allocation in research and development.
Ultimately, increased actuarial involvement can lead to increased competition, greater transparency, better-aligned incentives and improved mitigation of total cost of care increases over time. Let’s get going!
Statements of fact and opinions expressed herein are those of the individual authors and are not necessarily those of the Society of Actuaries or the respective authors’ employers.
References:
- 1. American Society of Gene & Cell Therapy. Gene and Cell Therapy FAQs. American Society of Gene & Cell Therapy (accessed March 15, 2020). ↩
- 2. Carbonell R., A. Mukherjee, J. Dordick, and C.J. Roberts. A Technology Roadmap for Today’s Gene Therapy Manufacturing Challenges. Cell & Gene, April 18, 2019. ↩
- 3. GeneTherapyNet.com. Viral Vectors. Gene Therapy Net (accessed June 2, 2020). ↩
- 4. U.S. Food & Drug Administration. Statement From FDA Commissioner Scott Gottlieb, M.D., and Peter Marks, M.D., Ph.D., Director of the Center of Biologics Evaluation and Research on New Policies to Advance Development of Safe and Effective Cell and Gene Therapies. U.S. Food & Drug Administration, January 15, 2019 (accessed December 11, 2020). ↩
- 5. Express Scripts. Evernorth Embarq Benefit Protection. Evernorth Health, Inc. (accessed December 11, 2020). ↩
- 6. Prime Therapeutics. Prime Therapeutics launches PreserverRx Gene Therapy Financial Protection. Prime Therapeutics, April 6, 2020 (accessed December 11, 2020). ↩
Copyright © 2021 by the Society of Actuaries, Chicago, Illinois.